How might we support the family caregiver in navigating the unknowns
of the University of Michigan Health System?
An estimated 1.3 million family caregivers in Michigan are actively supporting an ailing loved one. However, caregiving is hard. It is a new reality full of unknowns that is taxing on both body & mind. This project started out as a way to support family caregivers in navigating the unknowns of the University of Michigan Health System. In the process, we developed a story-based participatory approach which engaged patients, caregivers, clinical & non-clinical staff in designing better patient experiences. We codified this approach into a toolkit currently transforming the way the Office of Patient Experience (OPE) works.
Challenges included (1) building trust & credibility with our partner organization, OPE, and gaining access to groups within the system, (2) time constrains as clinicians have limited capacity to work on non-clinical tasks, and (3) navigating institutional barriers such as: system-wide hierarchies, slow implementation processes, and old-school mindsets that rely heavily on quantitative data as a means of improving patient experience.
The final deliverable ended up being a toolkit to support OPE project managers—Stories for Care uses the stories of patients & families as provocative data along with co-design activities to build multidisciplinary partnerships within the health system that promote patient and family-centered care. The toolkit provides an engagement framework and supporting activities for facilitating "Learn," "Do," and "Teach" co-design engagements aimed at developing interventions, procedures, and policies that build empathy for, and improve the experience of, patients & family caregivers in the health system.
Partners: Office of Patient Experience (OPE) at University of Michigan Health System
Role: integrative designer working with two integrative designers
Extent of the project: one and a half years, full-time
Recognition: Smucker Wagstaff Graduate Award (2017), Jean Paul Slusser Award for outstanding thesis (2018), Plantree International Conference Presenter (2018)
Tags: design research, problem-finding, human-centered design, design methods, innovation process, co-design, design toolkits, organizational transformation


Design Process.
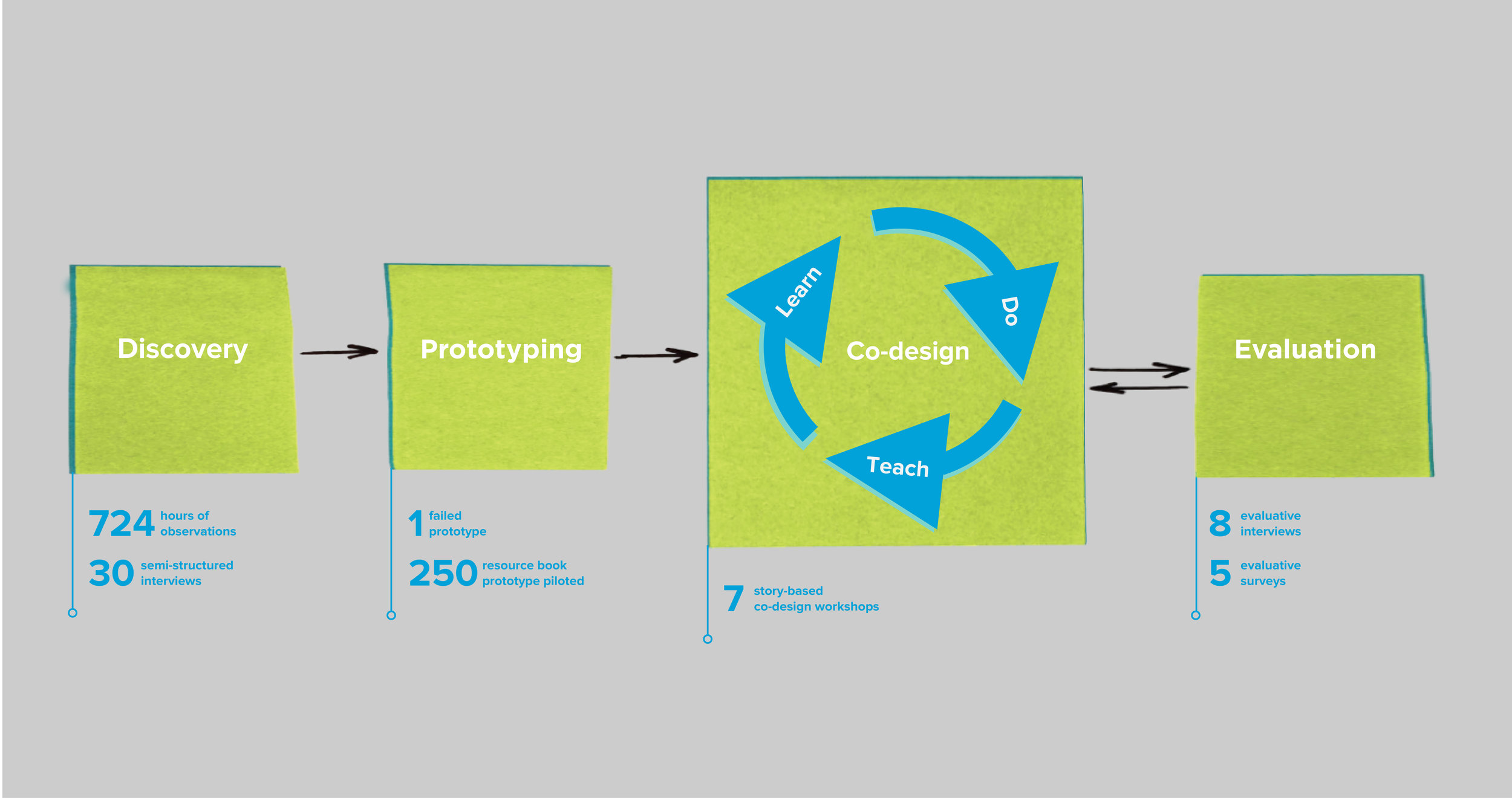
We spent several hundred hours in discovery research and then tested our assumptions by designing prototypes. The evaluation of the prototypes led us into a co-design process where we developed Learn, Do, and Teach co-design workshops. These workshops were evaluated, iterated upon, and codified into the Stories for Care Toolkit. While the design process is shown linearly, it was messy and had many iterative loops.
Discovery.
The OPE gave us an open-ended charge—find ways to improve patient experience in the health system. An extensive problem finding process led us to conclude that the family caregiver was a crucial touchpoint whose knowledge and contribution was lost in the system.
We conducted wide ranging ethnographic research, from following a pet therapy dog to observing a gastroenterological surgery. Our semi-structured interviews were not only with patients, caregivers, and clinicians, but we also spoke to environmental staff, housekeeping staff, and hospital security personnel who may be at the peripheries of the system, but have a huge impact on patient experience. Our problem-finding process included synthesizing our research into affinity maps, problem statements, personas, a service blueprint, and a stakeholder map.
A turning point in the research was when I followed a therapy dog and came across a family caregiver, a wife, of a critically ill patient who felt powerless—excluded from her husband's care and lacking ways that would allow her to participate in his care.
Such instances led us to develop the following insight:
Family caregivers desire to help their patients in any way they can, but are ill-prepared and poorly-supported to advocate for their patient. They feel a real or perceived inability to affect change in their loved one’s condition because they lack awareness of, or access to, tools that would allow them to participate in care more fully.
Process photo of us synthesizing interview & observation notes into a service blueprint of the family caregiver experience in the health system.
Prototyping & Evaluation.
Acting on insights, we developed a prototype for family caregivers that failed in an evaluation with nursing staff. Taking into account their feedback, we iterated to create a resource book for patients & caregivers. In piloting and evaluating the book we discovered a need for adopting a more participatory approach.
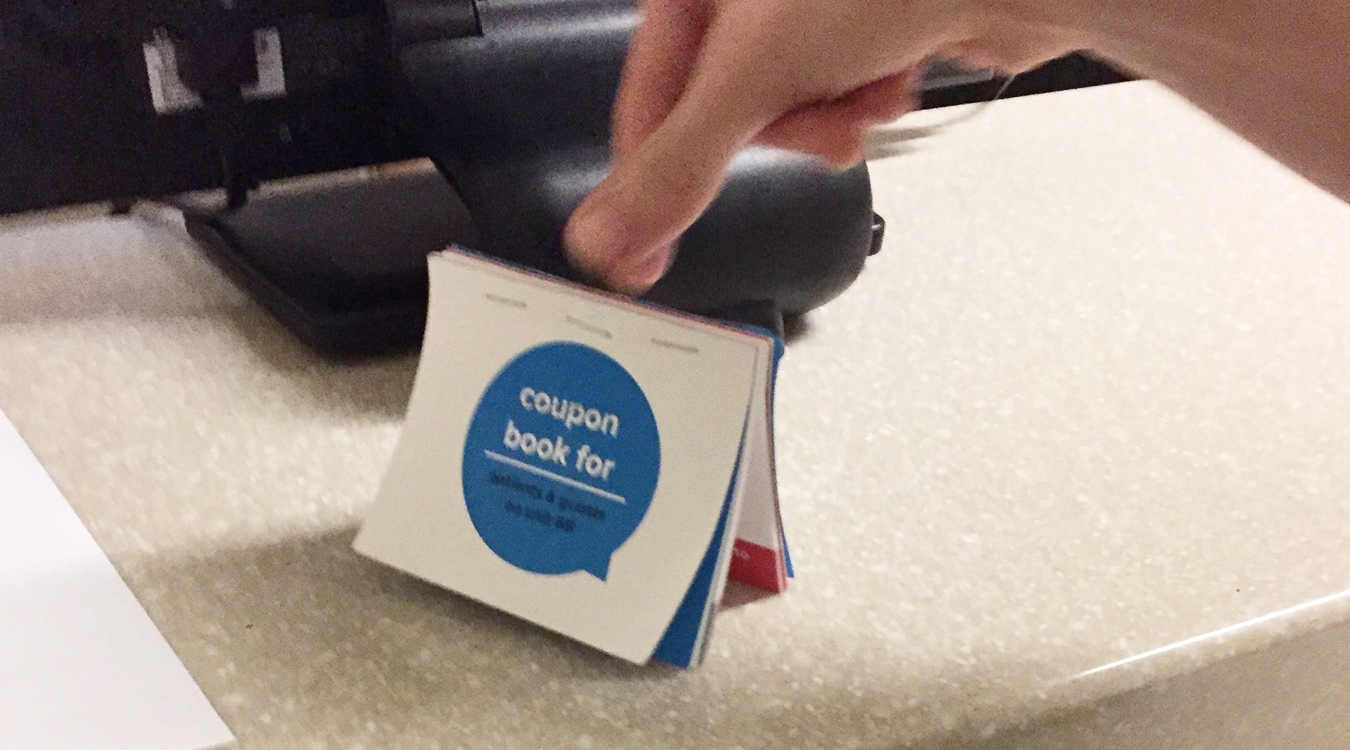
We brainstormed ways to bridge the gap between existing hospital resources and access to them. This led to the design of an intervention we nicknamed the “coupon book” that contained “coupons” redeemable by patients & family caregivers for resources like pet therapy and spiritual care. We wanted it to be a tool for both nursing staff & family caregivers, but in evaluations nurses found it transnational in nature. Iterating on the coupon book we developed the Need Something? Resource Book for Patients & Families that was friendly, accessible, and gave agency back to caregivers. We piloted & evaluated the book on a post-surgical unit in the hospital.
We piloted 250 copies of the resource book on a post-surgical unit in the adult wing of the hospital. We received encouraging feedback, but also noticed challenges in the delivery of the prototype. We realized we needed the help of nurse, patients, and caregivers in designing a more sustainable resource book—we needed to design with our end users.
Relevant quotes from our evaluative interviews of the resource book:
"I used it to call for spiritual counseling yesterday."
—patient on a post-surgical unit"Oh, wait...I think I remember. Was it in that folder? I don't really remember, I came in the middle of the night."
—patient on a post-surgical unit“I spent four hours with a patient going through the book. He was in a lot of pain. It was a nice distraction.”
—nurse on a post-surgical unit
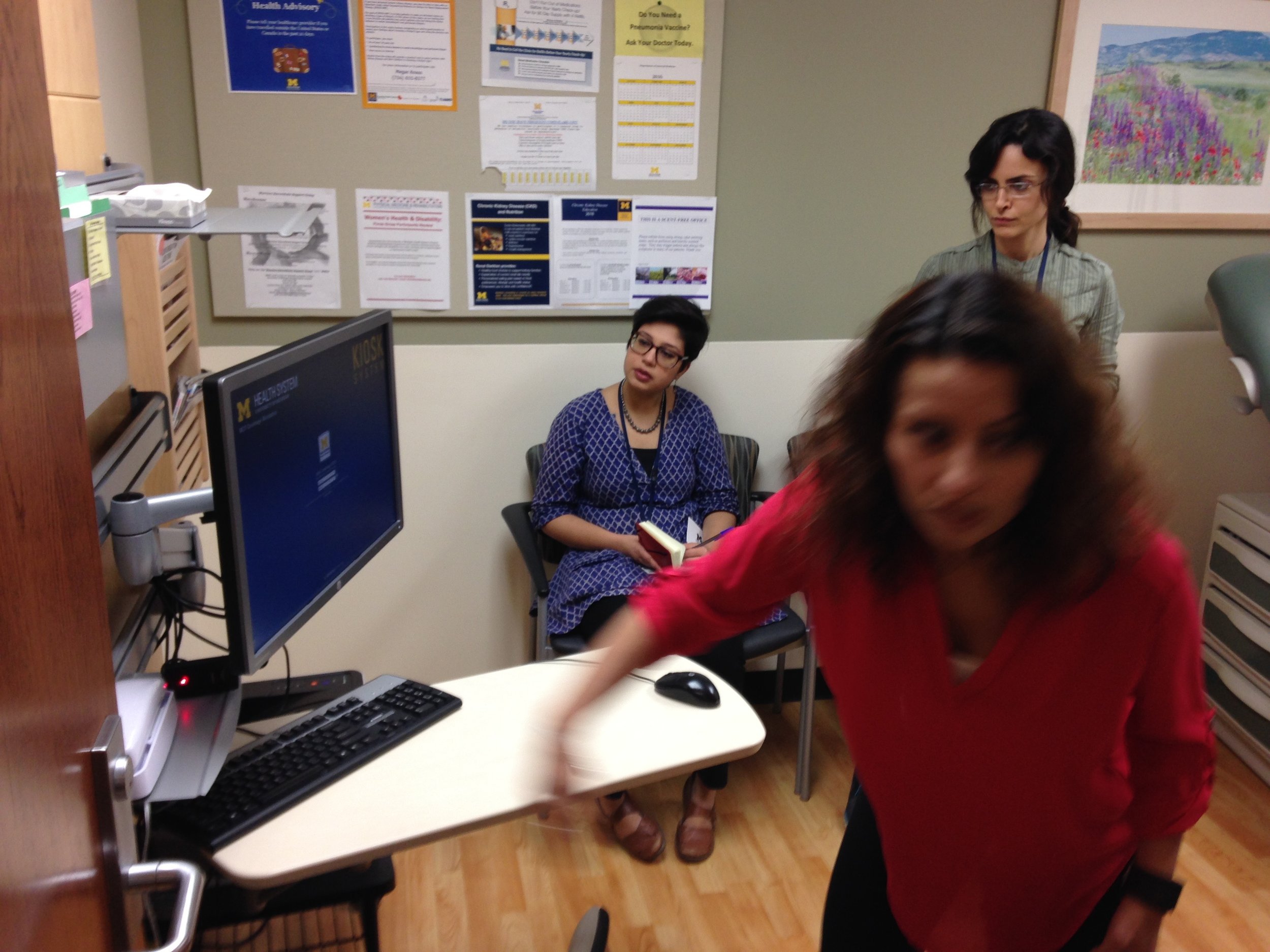
Photo from an evaluative interview with a 67-year old patient using the resource book.
Co-designing with Nurses, Caregivers, and OPE Staff.
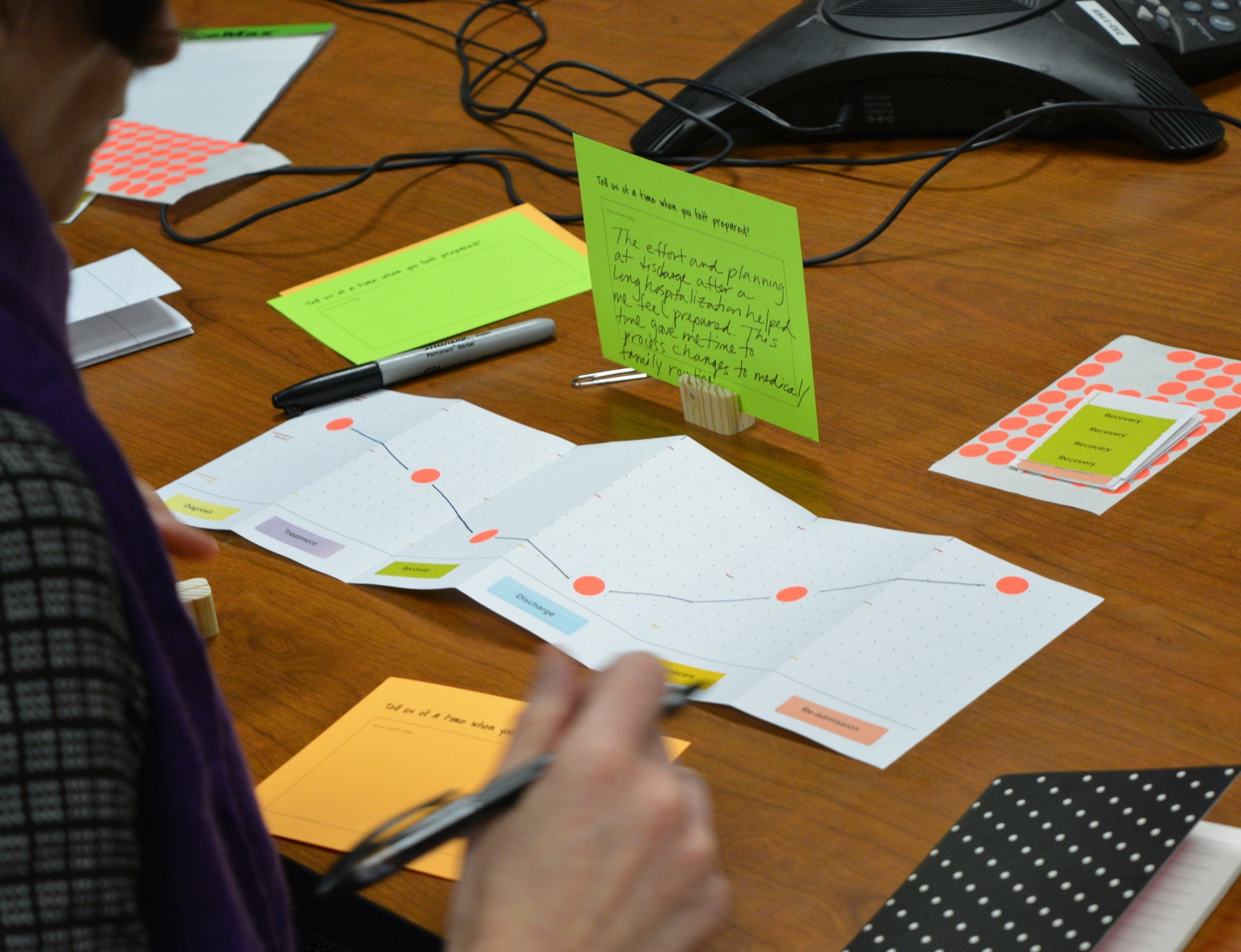
We created a series of story-based co-design workshops to make nurses & caregivers our partners in the design process. These workshops used stories from research as provocative prompts to channel participant creativity & problem-solving. We developed a framework from these workshops that was iterated upon into a toolkit.
We knew the limitations of the resource book as an intervention—it gave us insight into understanding the hierarchies within the health system. We learned that that any attempt at improving the caregiver experience was incomplete without the inclusion of the nursing perspective. We created a series of 45-60 minute workshops—Learn, Do, Teach—that used stories and design-led activities to provoke empathy, and prompt participants within the workshops to wrestle with the needs of the multiple actors within the story. The workshops became a more valuable outcome for us & our project partner—together we developed an engagement framework that became a toolkit.
Feedback from the workshops:
"This was on of the most fun and creative things I've done in a while"
—nurse in a Do workshop"I feel like stories highlights the human connection that is often lost in health system protocols and policies."
—family caregiver in a Learn workshop“From your workshop where a nurse says that the caregiver is worried about killing her husband—she realized that it is the caregiver's fear, it is the reality. It’s about building those high-quality connections. Bring in the human need. You have done it a higher level.”
—administrative director, OPE, on the workshops
The Stories for Care toolkit was born as an opportunity to support the OPE with design tools and processes to work more strategically within the health system and operationalize their approach. The organization was building in capacity and they needed to legitimate their approach, we took our knowledge about the health system along with the design tools we had created and merged them with OPE's approach to create the toolkit.
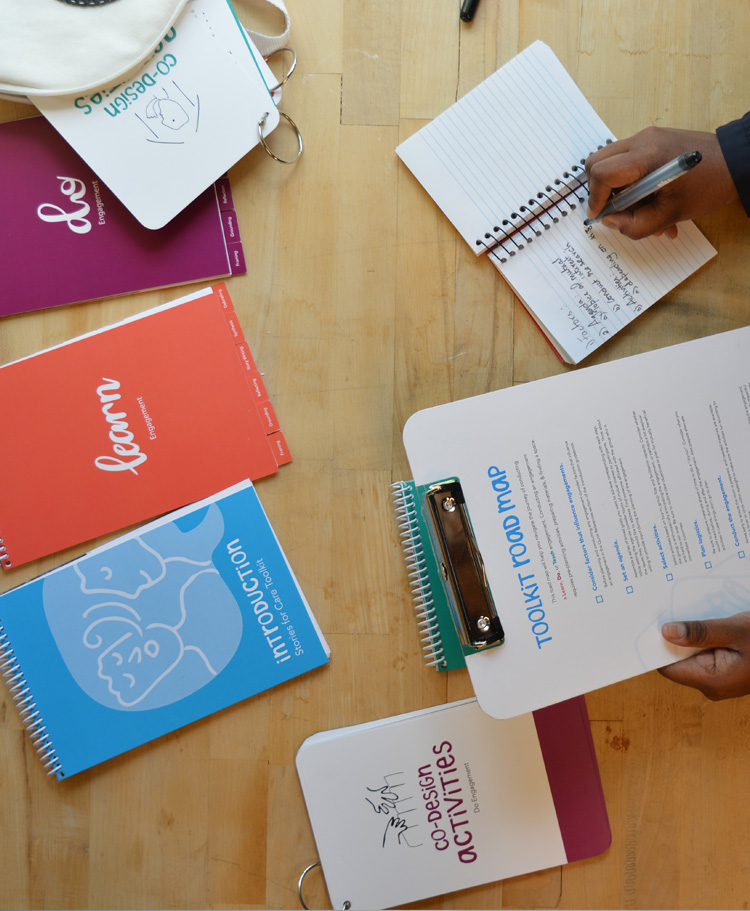
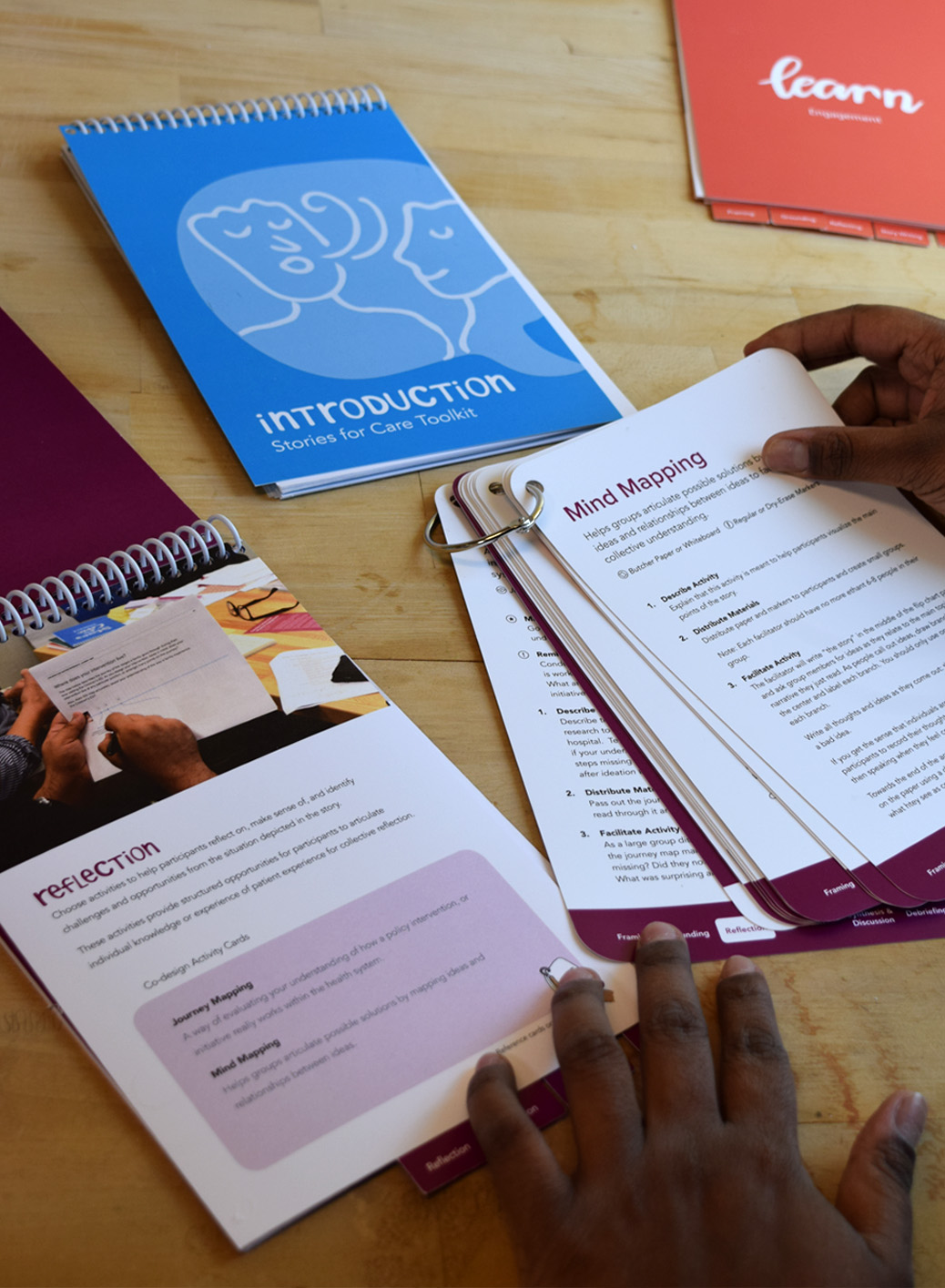
The Stories for Care toolkit includes the following:
- Introduction guide: introducing the toolkit, the engagement types, and the co-design process. It also includes a list of factors that influence engagements.
- Toolkit Road Map: a checklist for things to remember when designing and facilitating an engagement.
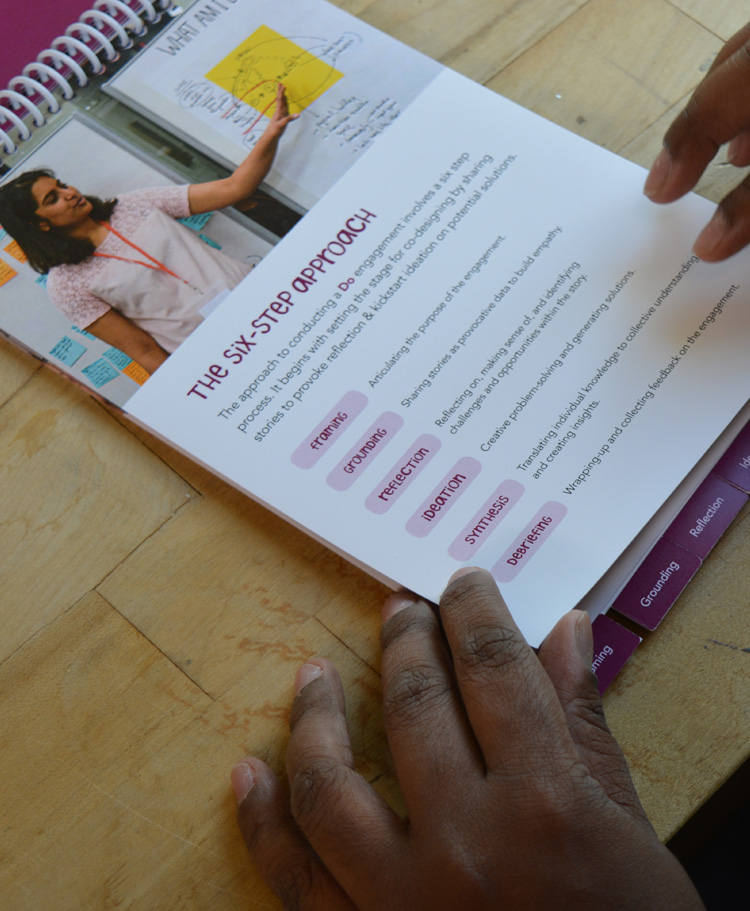
- Learn, Do, Teach guidebooks: provides goal & intended outcomes for each engagement type. They also provide a six-step approach for how to facilitate a Learn, Do, or Teach engagement.
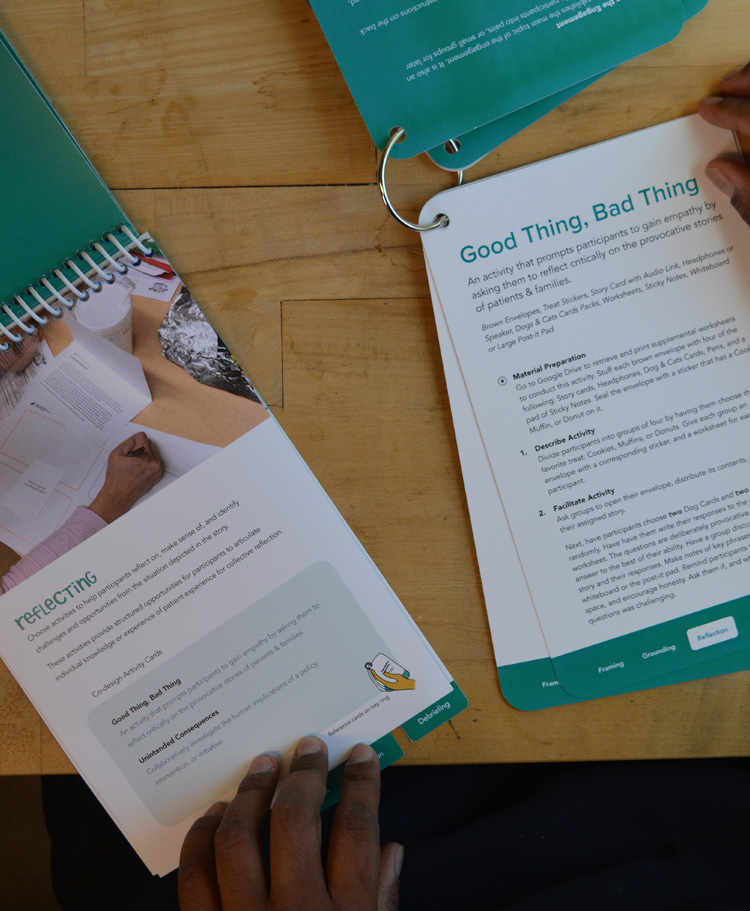
- Co-design activity cards: each set of cards provide instructions for how to facilitate co-design activities. They correspond with an engagement type.
- Google Drive folder: activity worksheets and other materials that can be easily modified and shared with colleagues.
We trained OPE project managers in how to use the toolkit, and it is currently being used with the University of Michigan Health System.
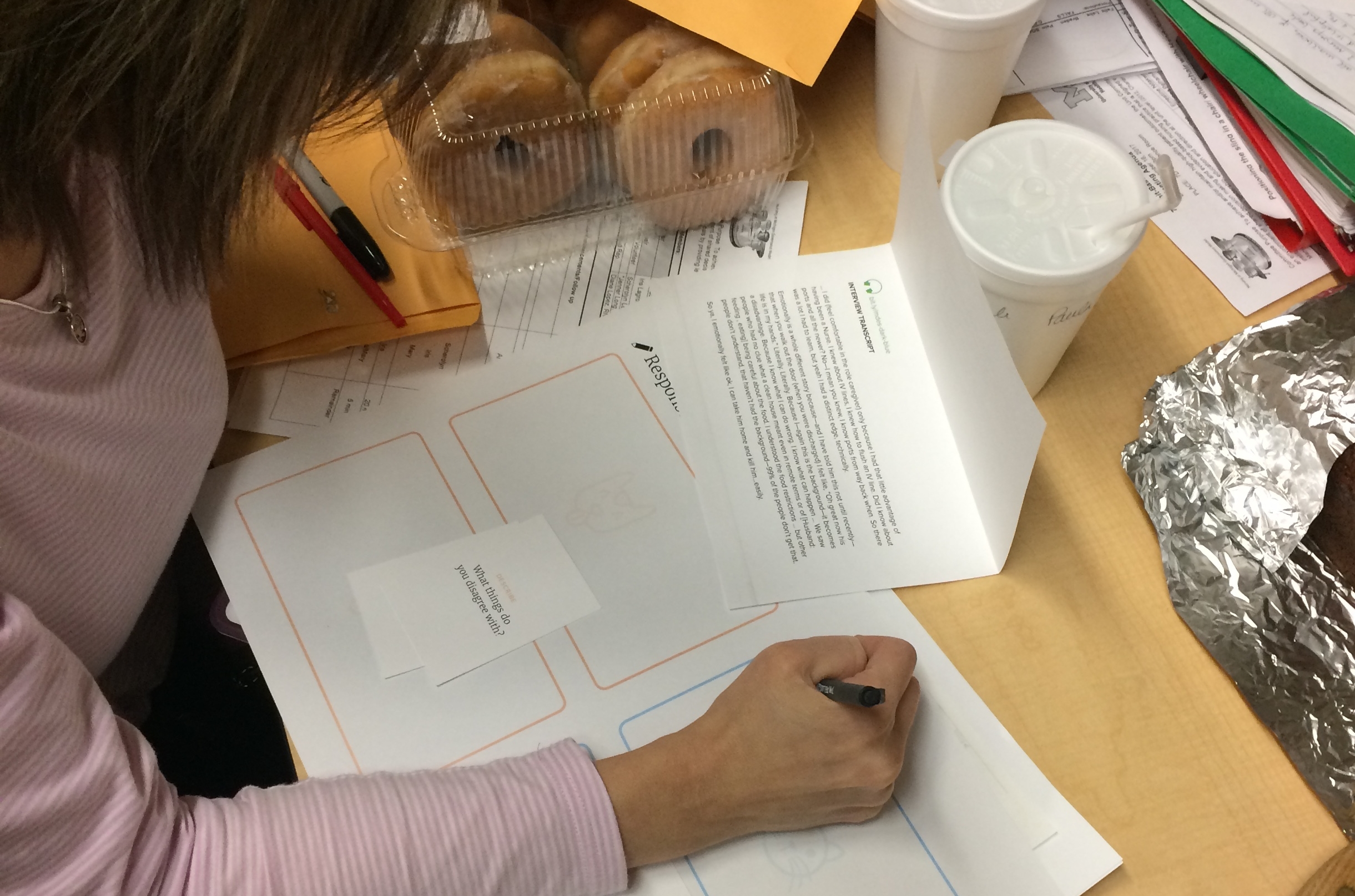
An exercise from a “toolkit translation” session where we worked with the OPE staff to translate our design terminology and language into the language they use to describe their work.
Photo with two team members handing off the Stories for Care toolkit to the Administrative Director and a project manager of the OPE.